Decidual Cast: Everything You Need to Know and When to See Your OBGYN

The female reproductive system is incredibly complex, and occasionally women experience unusual events that can feel alarming or confusing. One such rare occurrence is a decidual cast, which happens when a woman passes a large piece of uterine tissue that looks very different from typical menstrual blood or clots. This tissue is usually triangular in shape and can resemble a cast of the uterine cavity, which is why the phenomenon has earned the name “decidual cast.”
Although decidual casts are rare, awareness has grown in recent years, partly due to social media posts where women share their experiences. While seeing a decidual cast can be shocking, it is usually not life-threatening. However, because it may reflect hormonal shifts or other underlying reproductive conditions, it’s important to consult an experienced OBGYN if you experience this. Understanding the causes, symptoms, and management options can help women feel informed and reassured.
What is a Decidual Cast?
A decidual cast occurs when the entire endometrial lining of the uterus (decidua) sheds at once rather than gradually, passing as a single piece or in large fragments. Unlike a normal period, where the uterine lining sheds over several days in small amounts, a decidual cast can maintain the three-dimensional shape of the uterine cavity, often triangular or sac-like, sometimes extending up to several inches in length. The tissue consists of decidualized endometrium, which develops in response to progesterone during the menstrual cycle or early pregnancy. When expelled, the tissue is usually pink to reddish-gray, with a fleshy, spongy texture. Its appearance can be alarming, especially for women who are unfamiliar with the condition.
The term “decidual” refers to the thickened endometrial tissue, while “cast” reflects its shape as it passes through the cervix and vagina. Decidual casts have been documented in medical literature for centuries, but they remain relatively uncommon, and awareness among women and some healthcare providers is limited.
While the phenomenon may look concerning, decidual casts are generally benign, though they may point to underlying hormonal changes or other reproductive health issues that should be evaluated by a qualified OBGYN.
How Does a Decidual Cast Form?
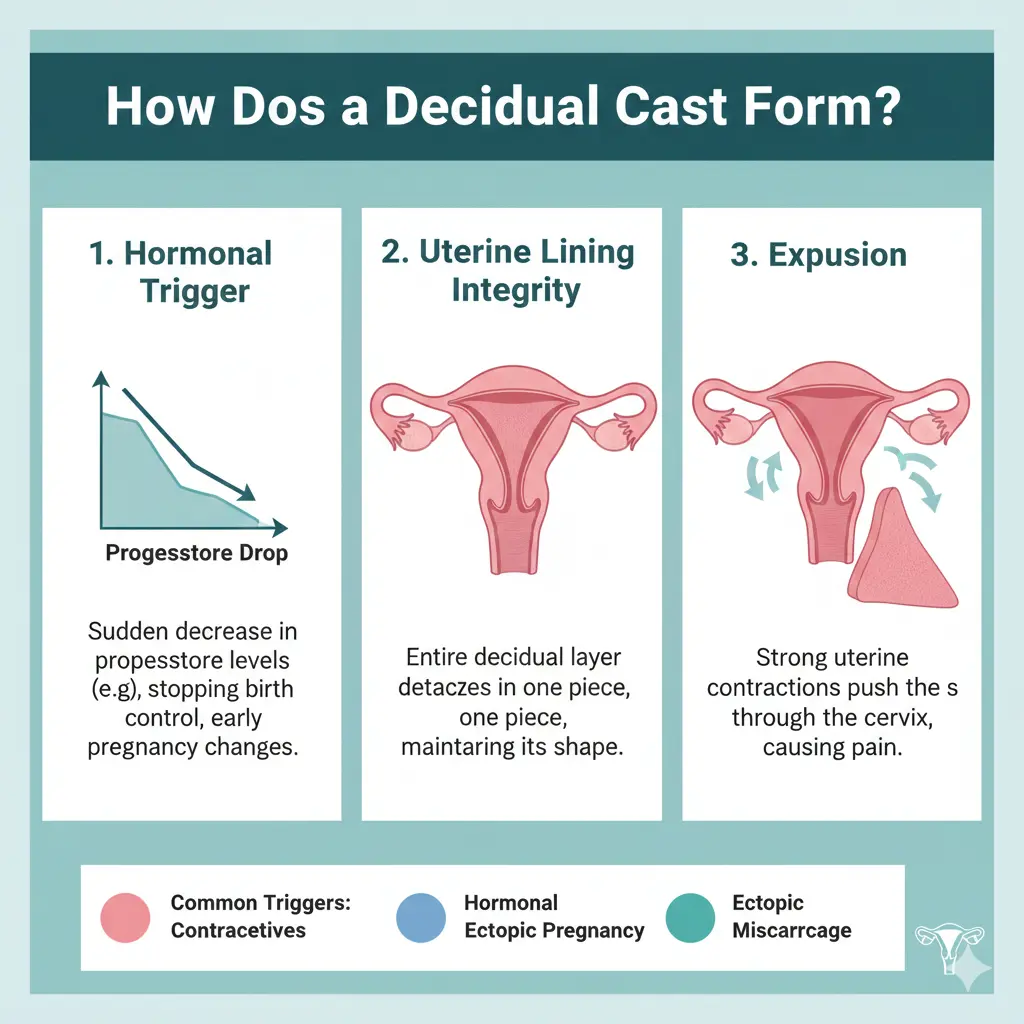
To understand how a decidual cast forms, it’s important to know a bit about the menstrual cycle. Each month, the endometrium thickens in preparation for a potential pregnancy under the influence of hormones, especially progesterone. Normally, if pregnancy doesn’t occur, this lining gradually breaks down and is shed over several days during menstruation.
In the case of a decidual cast, the entire lining sheds at once, often due to a rapid drop in progesterone or sudden hormonal fluctuations. This can happen in several contexts:
- During a normal menstrual cycle when hormone levels change unpredictably.
- Following changes in hormonal contraception, such as stopping birth control pills, removing hormonal IUDs, or discontinuing injectable contraceptives like Depo-Provera.
- In early pregnancy if hormonal support is inadequate or if there is an early pregnancy loss.
Certain medications, including fertility treatments or hormone therapy, may also influence the development and shedding of the endometrium, increasing the likelihood of a decidual cast.
Reproductive conditions such as PCOS, adenomyosis, endometriosis, or ectopic pregnancy can also alter the hormonal environment in the uterus, potentially triggering a decidual cast. In rare cases, inflammatory or infectious processes affecting the reproductive tract may play a role.
While the exact cause can vary, the common link is usually a sudden hormonal change that leads to the synchronized shedding of the uterine lining.
Common Causes of Decidual Cast
Several factors can contribute to the formation of a decidual cast. Understanding these can help women and healthcare providers determine whether the event is isolated or indicative of an underlying condition.
Hormonal Fluctuations
The most common trigger is a sudden change in progesterone levels. Progesterone is essential for thickening the uterine lining in preparation for implantation. A rapid drop, whether natural or medication-induced, can cause the endometrium to shed all at once. This explains why decidual casts sometimes occur after stopping hormonal contraceptives or other progestin-containing treatments.
Hormonal Medications
Hormonal treatments, including contraceptives, fertility therapies, and hormone replacement therapy, can influence endometrial development. Synthetic hormones can create a lining that is thicker or sheds differently than the body’s natural cycle, making decidual casts more likely in some women.
Reproductive Health Conditions
- Polycystic Ovary Syndrome (PCOS): Irregular hormone patterns can trigger unusual endometrial shedding.
- Endometriosis: Can influence uterine lining behavior and cause heavy or irregular shedding.
- Adenomyosis: Thickened uterine lining can lead to more extensive tissue passage.
- Early Pregnancy Loss or Ectopic Pregnancy: Tissue may appear similar to a decidual cast but often requires urgent medical evaluation.
Other Potential Factors
Some studies suggest links between decidual casts and inflammation or infection, though these are less common. Regardless of cause, medical evaluation is important to rule out complications.
Symptoms and Signs
The most distinctive feature of a decidual cast is the passage of tissue that maintains the uterine cavity’s shape. Key characteristics include:
- Shape: Triangular or inverted triangle, sometimes resembling a mold of the uterus.
- Size: Typically 1–4 inches long.
- Color: Pink to reddish-gray, fleshy, sometimes spongy.
- Consistency: Firm enough to hold its shape, unlike regular menstrual clots.
Women often experience moderate to severe cramping, usually more intense than normal menstrual cramps, as the uterus contracts to expel the tissue. Other symptoms may include:
- Vaginal bleeding, ranging from light spotting to heavier flow.
- Lower abdominal pain.
- Nausea or occasional vomiting due to pain intensity.
- Temporary fatigue or discomfort during and after passage.
Timing may vary: it can occur during a normal period, between periods, or after hormonal changes. The entire event often resolves within 24 hours, though lingering discomfort and bleeding may continue for a few days.
It is common for women to mistake a decidual cast for a miscarriage or other serious condition, which can cause significant anxiety.
When to See Your OBGYN
While a decidual cast is generally not an emergency, certain circumstances require prompt medical attention:
- Heavy bleeding (soaking a pad or tampon every hour for 2+ hours).
- Severe abdominal pain that doesn’t subside after passage.
- Fever or foul-smelling discharge indicating possible infection.
- Dizziness or fainting, suggesting significant blood loss.
- Tissue passage after a positive pregnancy test.
Even in the absence of alarming symptoms, scheduling a visit with an OBGYN is recommended. Professional evaluation can confirm that the tissue is a decidual cast rather than pregnancy tissue or a complication, provide reassurance, and identify underlying causes if needed.
Must Visit: 30 Day Water Fast: Benefits, Body Changes, Risks, Safety, and What Experts Say
Women who experience recurrent decidual casts may require a more in-depth hormonal or reproductive evaluation to prevent future episodes.
Diagnosis of Decidual Cast
A thorough evaluation usually includes:
Medical History and Physical Exam
- Recent menstrual and hormonal history.
- Any medications, especially hormonal treatments.
- Symptoms before, during, and after the event.
Laboratory Testing
- Pregnancy test to rule out early pregnancy or miscarriage.
- Hormone panels to check for imbalances (estrogen, progesterone, thyroid hormones).
- Complete blood count (CBC) if significant bleeding occurred.
Tissue Analysis
If possible, preserve the tissue for pathological examination. This helps confirm a decidual cast and distinguish it from other types of tissue, such as miscarriage tissue.
Imaging
- Transvaginal ultrasound to examine uterine lining and identify any retained tissue.
- Sonohysterography (SIS) or hysteroscopy may be used for recurrent cases or structural concerns.
Through these evaluations, an OBGYN can develop a tailored care plan, ensure nothing serious is missed, and provide reassurance.
Read Also: Rupa Health: Revolutionizing Lab Testing and Personalized Medicine
Treatment and Management
For most isolated cases, treatment is focused on comfort and symptom management:
Pain Relief
- Over-the-counter medications like ibuprofen or naproxen help with cramping and may reduce bleeding.
- Severe pain may require short-term prescription medications.
Hormonal Management
- If the cast is related to hormonal contraception changes, an OBGYN may recommend adjusting the method or tapering hormones gradually.
- For recurrent issues, hormonal therapy may be used to stabilize the endometrium.
Addressing Underlying Conditions
- Conditions like PCOS, endometriosis, or adenomyosis may require ongoing treatment.
- Individualized plans can prevent recurrent decidual casts and improve overall reproductive health.
Most women recover fully without long-term complications, and bleeding usually resolves within a few days.
Prevention and Long-Term Considerations
Although decidual casts cannot always be prevented, some strategies may reduce the risk:
- Gradual transitions when starting or stopping hormonal medications.
- Lifestyle measures to maintain hormonal balance: regular exercise, proper sleep, stress management, and nutrition.
- Regular OBGYN check-ups to monitor reproductive health.
- Tailored approaches for women with recurrent decidual casts, including hormonal regulation and management of underlying reproductive conditions.
Ongoing care ensures early detection of any issues and helps maintain overall reproductive well-being.
Real Experiences and Patient Guidance
Women who experience a decidual cast often report shock and anxiety due to the unusual appearance of tissue. Sharing experiences on social media or with healthcare providers can normalize the experience and reduce fear.
Practical guidance includes:
- Preserve the tissue in a clean container if possible.
- Take photos if unable to preserve the tissue.
- Record timing, symptoms, and any recent medication changes.
- Schedule an appointment with an experienced OBGYN.
Understanding the condition helps women feel informed, reduces anxiety, and ensures appropriate follow-up care.
Conclusion
A decidual cast is a rare but generally non-dangerous reproductive event where the uterine lining sheds in one piece or large fragments. While it can appear alarming, most cases resolve naturally. However, medical evaluation is important to rule out complications, confirm the diagnosis, and address underlying causes if needed.
Women experiencing this event should consult an OBGYN for reassurance, evaluation, and personalized guidance. Awareness, proper care, and professional support can help women navigate this uncommon phenomenon with confidence and maintain long-term reproductive health.
If you believe you have passed a decidual cast or notice unusual tissue during your cycle, contact your OBGYN promptly. Professional evaluation provides clarity, peace of mind, and ensures that you receive appropriate care for your reproductive health.